
Table of Contents
Burnout rates among physicians are distressingly high, according to numerous studies. High productivity goals, EHR documentation tasks, long working hours, time pressures, and difficulty balancing work and life are among the major factors contributing to the rising level of physician burnout. Medical transcription outsourcing helps reduce physician burnout by allowing them to focus on patient care instead of documentation. Today, AI-driven virtual healthcare assistants are changing the game.
Surveys Reveal High Stress Levels Among Physicians
Survey data from the American Medical Association (AMA) shows that 51% of physicians experienced burnout in 2022, up from previous levels. An athenahealth survey by Harris Poll found that nearly all U.S. physicians report feeling regularly burned out, with over half considering leaving the profession or moving into non-patient-facing roles.
The MEMO (Minimizing Error, Maximizing Outcome) Study, funded by the AHRQ, found that over half of primary care physicians experience stress due to time pressures and challenging work conditions. The study also revealed that the anticipated stress relief from implementing electronic health records (EHRs) has not materialized; instead, EHR adoption can contribute to burnout. Researchers observed that practices implementing EHRs initially saw an increase in stress, which eventually declined as EHR use matured—but stress levels never returned to baseline. Moreover, fully integrated EHR systems, especially in practices with shorter visit times, were linked to increased physician stress, burnout, and even intentions to leave the profession.
Chicago-based Rush University System for Health experiments with AI Assistant Experiment
A report from Fierce Healthcare published in April 2024, noted that a growing number of hospitals and health systems are leveraging advancements in AI to help address the challenges faced by physicians. The report highlights Chicago-based Rush University System for Health’s trial of an AI healthcare assistant aimed at reducing the time clinicians spend on EHR documentation and other tasks.
The Chicago-based Rush University System for Health, which includes several medical centers and outpatient facilities, is partnering with technology company Suki to pilot its AI assistant. The trial will begin with a “few hundred” physicians, with plans to gradually expand the technology to more providers.
In addition to ambient note generation, Suki offers Siri-like dictation features, coding, and answering capabilities via data retrieval. The company reports that its solution enables clinicians to complete notes an average of 72% faster. It also highlights additional benefits for health systems, including a 48% reduction in amended encounter rates, a substantial decrease in claim denials, and opportunities for incremental revenue generation, and improved operational efficiencies.
How AI Transforms EHR Documentation and Reduces Physician Burnout
AI-driven virtual healthcare assistants transform EHR (Electronic Health Record) documentation by automating and streamlining tasks that healthcare providers take substantial time and effort to complete.
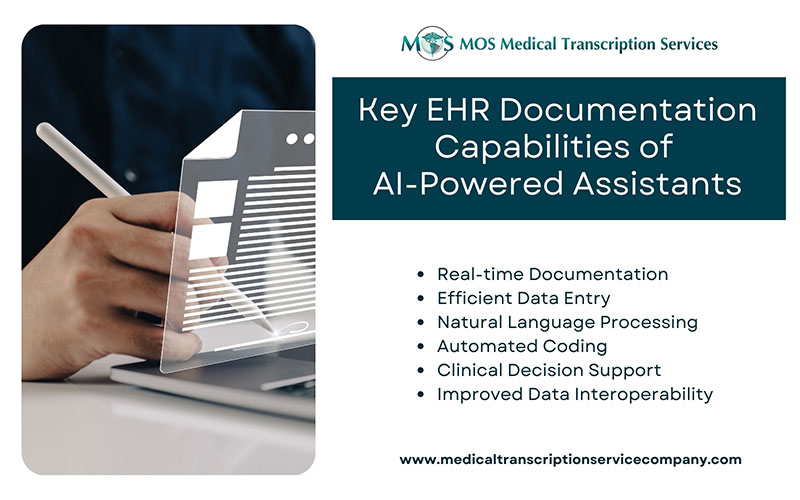
The key EHR documentation capabilities of AI-powered assistants include:
- Real-time documentation: Virtual assistants leverage voice recognition technology to capture clinical notes and patient interactions in real-time. This minimizes manual input and helps ensure that patient records are accurate, complete, and up-to-date.
- Efficient data entry: By collecting and synthesizing information from multiple sources, virtual healthcare assistants reduce the EHR data entry load on healthcare providers. By automating tedious data entry, physicians can save up to two hours a day, according to linda.ai. These assistants can even pull data from lab reports, imaging results, and patient histories to provide a more complete record without additional steps.
- Natural Language Processing (NLP): Using NLP, AI tools can understand and categorize medical language, including terminology of various medical specializations. This allows them to accurately interpret clinical information, organize it logically, and structure it according to EHR requirements. As a result, they can transform patient consultations into EHR entries in a flash. NLP can analyze large amounts of medical data, detect errors, and help clinicians make timely decisions by providing access to complete patient data.
- Automated coding: AI-driven assistants can automatically suggest accurate coding for diagnoses, procedures, and treatments, improving the quality of documentation and supporting compliance. This feature reduces coding errors, which can help prevent claim denials and improve revenue cycle outcomes.
- Clinical decision support: Some advanced virtual assistants offer decision-support features by analyzing patient data. AI can help clinicians make more informed decisions about patient care through clinical decision support (AI-CDS) systems. They help reduce diagnostic errors and medication errors, and offer insights or reminders for evidence-based care, which can be directly added to the EHR as actionable items for the provider.
- Improved data interoperability: These AI tools can facilitate interoperability. By integrating data from different systems, AI ensures that providers have access to a comprehensive view of a patient’s health history across various platforms and care settings. AI interoperability ensures that healthcare providers can interpret patient information accurately and efficiently, regardless of the system or format in which the data was originally recorded. When providers have access to comprehensive and accurate patient information across different systems, it leads to better diagnosis, treatment, and patient outcomes.
With all of these capabilities, AI-driven virtual healthcare assistants help reduce physicians’ administrative burden, a major contributing factor to burnout. AI tools improve the quality of patient data in EHRs, and create more efficient workflows, enhance focus on patient care and alleviate physician burnout.
Ensuring Accuracy in Medical Documentation: The Value of Human Expertise
However, while NLP can be very useful, it is not possible to guarantee complete accuracy. Computers may struggle with spelling errors, grammatical errors, abbreviations, and unique or unconventional phrases that are common in medical documentation. These challenges can lead to inaccuracies that may impact the quality and reliability of patient records. A medical transcription company, staffed with skilled professionals, can bridge this gap by providing the expertise needed to correctly interpret and transcribe complex medical language, ensuring that the documentation is precise, clear, and aligned with medical standards. Their support helps maintain the integrity of patient records, improves the workflow for healthcare providers, and ultimately contributes to better patient care.


