Table of Contents
Around one in five American adults experience a mental health condition each year, according to the National Institute of Mental Health. As the demand for care grows, efficient behavioral health documentation has become more important than ever. Providers also rely on medical transcription services to maintain clear, accurate, and complete patient records and support behavioral health record keeping as part of routine care.
A 2023 study published by the JAMA Health Forum highlighted how much mental health care use has increased. For providers, this makes high-quality and up-to-date documentation essential. Good documentation supports medical necessity, coding, billing, and continuity of care. It also helps behavioral health specialists stay focused on their patients while delegating parts of the documentation process to trained professionals. This also reflects why high-quality documentation is important in behavioral health in the current care environment.
Significance of Behavioral Health Documentation
The importance of clinical documentation in mental health treatment lies in its ability to track patient progress, drive compliance, and promote measurable outcomes in today’s value-based care environment. Providers are no longer evaluated on the volume of services delivered, but on how effectively those services improve a patient’s symptoms, stability, and quality of life.
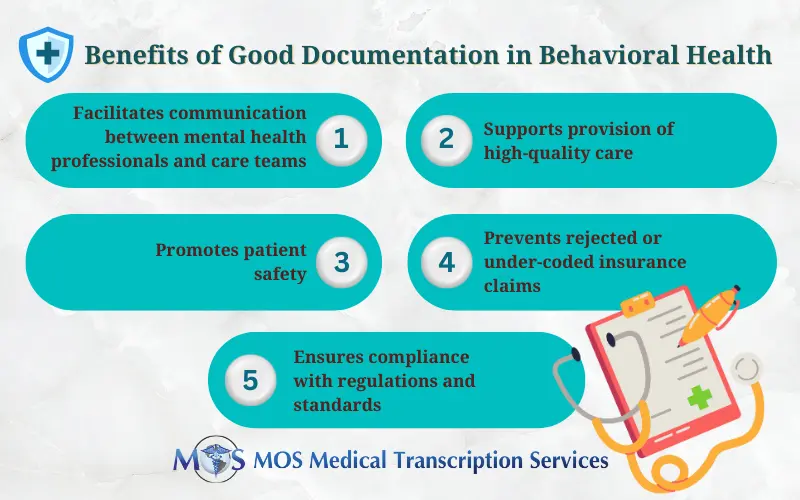
Strong mental health documentation practices are essential to:
- Reflect medical necessity: Strong documentation ensures treatments are justified and meet payer requirements.
- Track patient progress: Accurate records help monitor symptoms, response to treatment, and care outcomes.
- Support evidence-based decisions: Detailed notes guide clinicians in making informed, data-driven treatment choices.
- Reduce claim denials: Comprehensive documentation strengthens claims and minimizes the risk of reimbursement issues.
- Enhance care coordination: Multidisciplinary teams have access to timely, accurate information for consistent patient care.
- Protect patient safety: Complete records during crises or clinician transitions preserve critical clinical history.
- Facilitate informed handoffs: New providers can make decisions without missing context or gaps.
- Capture clinical reasoning: Notes detail risk assessments, treatment decisions, and clinical rationale, protecting both patients and providers.
Beyond clinical value, meeting behavioral health compliance requirements protects providers against audits, legal risks, and reimbursement disputes. Clear, defensible records outline clinical reasoning, risk assessments, and treatment decisions—protecting both patients and clinicians.
Trends in Mental Health Illness Prevalence and Service Use
The use of behavioral medicine services has increased along with the rising prevalence of “any mental illness” (AMI) and “serious mental illness” (SMI). Reports from the National Institutes of Health highlight important findings:
- Mental health service use increased by 39% from March 2020 to August 2022.
- AMI was more common among females (27.2%) than males (18.1%).
- Young adults aged 18–25 years had the highest prevalence of AMI at 33.7%, compared to 28.1% for ages 26–49 and 15% for ages 50+.
- In 2021, SMI affected 14.1 million adults (5.5% of all adults).
- Among the 57.8 million adults with AMI in 2021, 26.5 million (47.2%) received mental health services.
Research from RAND published in August 2023 showed that mental health service use increased by 22% during the early phase of the pandemic. While in-person visits dropped by 40%, tele-mental health visits increased ten-fold compared to the previous year.
These studies covered anxiety disorders, major depressive disorder, bipolar disorder, schizophrenia, and PTSD. As study coauthor Dena Bravata noted, the rising demand highlights the need to integrate behavioral health into primary care. This integration can help improve access, reduce stigma, and support a more comprehensive approach to patient well-being.
Ensure Comprehensive and Precise Documentation
Behavioral health practices must keep complete and accurate documentation for every patient encounter. This includes documenting the medical necessity behind each service provided. From the first visit onward, several types of records must be clear, detailed, and aligned with clinical standards.
- Intake and Assessment: Accurate intake and assessment documentation helps support a proper diagnosis. It should include a detailed diagnostic evaluation, clinical interview, and psychiatric assessment. Providers should also rule out alternative diagnoses.
Essential information to document includes:
- Presenting concerns
- Mental health history
- Previous treatments
- Current healthcare providers
- Demographics
- Medications
- Substance use details
- Physical and mental health conditions
This section should also include descriptions of current medications, treatments, assistive devices, and any past medication side effects.
- Treatment Plan: A strong treatment plan outlines the patient’s diagnosis, goals, objectives, interventions, and treatment options. It should also specify the treatment modality, session frequency, and how progress will be measured over time.
- Ongoing Care: If a patient needs a referral or a transfer to another provider, clear documentation is essential. This includes details of the informed-consent discussion, reasons for the change, and confirmation that the patient understands their rights. Documenting the potential benefits and risks of new programs or services is also important.
- Transferring Care: Accurate progress notes support proper billing, reimbursement, and overall care. These notes can also be used by other providers involved in the patient’s treatment. These notes should include demographic information, subjective and objective descriptions of client behavior, their symptoms, a summary of their diagnosis, what the client discussed in each session, your professional opinion, a treatment plan, and referrals if necessary. Be sure to record details such as:
- The basis for the referral or transfer
- The specific provider or program the patient is being referred to
- The important points covered in the informed consent conversation
- The patient’s agreement to go ahead with the referral/transfer
- Discharge Summary: When treatment is complete, a discharge summary should be prepared and signed by both provider and patient. This summary must include the final diagnosis, reason for discharge, progress toward treatment goals, any safety risks, and helpful post-discharge resources or referrals.
Best Practices for Clinical Documentation
Keep the following guidelines in mind to ensure strong documentation:
- Use progress notes and treatment plans to show changes in the patient’s condition.
- Maintain consistency across all records to create a complete clinical picture.
- Keep all clinical notes confidential.
- Always include the date and time of documentation.
- If corrections are made, explain the reason and update all related records.
- Avoid vague wording; use clear, objective language.
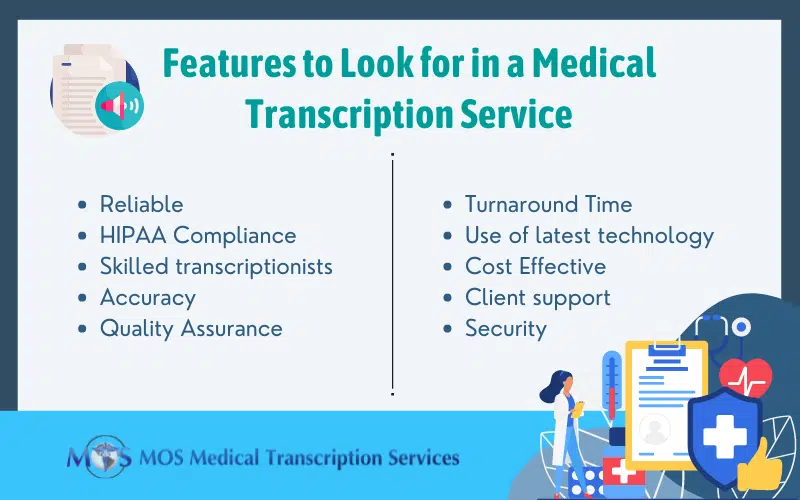
Contracting out mental health transcription tasks is an effective way to strengthen documentation quality. By relying on AI-integrated medical transcription services, behavioral health providers can ensure accurate and structured records that meet clinical and legal standards. Automatically generated reports are carefully reviewed by human transcriptionists to ensure they are error-free. A professional medical transcription company can deliver organized, legible, and complete HIPAA-compliant SOAP, DAP, EMDR, intake notes, enabling behavioural health specialists to spend less time managing documentation and focus on patient care.