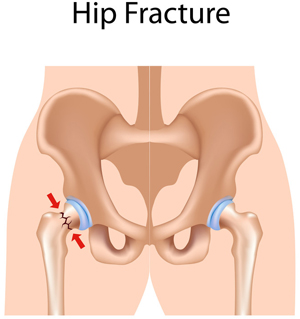
 Most often, hip injuries get little attention compared to injuries to the knee, ankle and shoulders due to their low prevalence. However, you should document hip fractures accurately through effective orthopedic transcription for the proper management of these types of fractures. Improperly managed injuries may result in severe consequences. There are several potential complications associated with intracapsular hip fracture (femoral neck) and extracapsular hip fracture (intertrochanteric, subtrochanteric).
Most often, hip injuries get little attention compared to injuries to the knee, ankle and shoulders due to their low prevalence. However, you should document hip fractures accurately through effective orthopedic transcription for the proper management of these types of fractures. Improperly managed injuries may result in severe consequences. There are several potential complications associated with intracapsular hip fracture (femoral neck) and extracapsular hip fracture (intertrochanteric, subtrochanteric).
Significance of History and Physical Examination Report
The correct diagnosis of hip fracture is done with a detailed history, a thorough physical examination and plain-film radiographs of the symptomatic hip. Physical examination would reveal an abducted and externally rotated hip with leg-length discrepancy with patients having severe hip pain and unable to walk. Hip fracture patients with vague pain in their buttocks, knees, thighs, groin, or back frequently report no antecedent trauma, especially when cognitive impairment is present and their physical examination (assessments of active, passive, and resisted movements of the affected hip joint and limb) may be normal. Based on this, diagnostic studies can be conducted to confirm any complications. If the radiographic findings only give the suspicion of a hip fracture, other imaging modalities can be used for confirming the diagnosis. The potential complications associated with each type of hip fracture are as follows.
Femoral neck
- Avascular necrosis of the femoral head
- Nonunion or malunion
- Late degenerative changes
Intertrochanteric
- Rarely, nonunion or malunion
- Degenerative changes
Subtrochanteric
- High rates of nonunion and implant (intramedullary nails or devices)
- Fatigue due to high physical stress in the region
History and physical examination report includes history of present illness, review of past history, and detailed results of physical examination and diagnostic studies. Physicians can understand the symptoms of the hip fracture better with this report and determine whether there are any severe complications. This will enable them to provide appropriate treatment to manage the fractures more effectively.
Managing Hip Fractures in the Elderly
The new guidelines from the American Academy of Orthopedic Surgeons (AAOS) provide several recommendations to manage hip fractures in patients aged above 65. The recommendations supported by strong evidence are as follows.
- Regional analgesia can be used to enhance preoperative pain control in patients having hip fracture.
- If the patient is undergoing hip fracture surgery, similar outcomes can be achieved using general or spinal anesthesia.
- Arthroplasty should be used in the case of patients having unstable (displaced) femoral neck fractures.
- Use of a cephalomedullary device for the treatment of patients having subtrochanteric or reverse obliquity fractures.
- A blood transfusion threshold of no higher than 8g/dl should be used in asymptomatic postoperative hip fracture patients.
- Intensive post-discharge physical therapy enhances functional outcomes.
- Use of an interdisciplinary care program in hip fracture patients having mild to moderate dementia enhances functional outcomes.
- Multimodal pain management should be used after hip fracture surgery.
You should prepare appropriate documentation while utilizing any of these recommendations for the management of hip fractures. For example, you should properly document patient assessment, admission notes, history and physical notes, or consultation notes when it comes to providing anesthesia. The other complications of elderly patients with hip fractures should be documented as well. For example, acute confusional state (ACS) is a common and severe complication in elderly people treated for femoral neck fractures, which should be documented well. If you are a busy practitioner/healthcare facility, you can rely upon medical transcription services to handle enormous documentation related to hip fracture and save your valuable time.


