Medical records are essential documents that provide details about the patient’s history, clinical findings, results of laboratory tests, pre- and postoperative care and more. Like any other specialty, dental practices should also maintain accurate patient records that reflect the quality of service provided and how the treatment plan is progressing. Professional medical transcription services can help practices maintain reliable patient records.
Table of Contents
Dental records include all details such as – medical history, diagnostic information, clinical notes, treatment plan, and patient-related communications that occur in the dentist’s office, including instructions for home care, consent to treatment, and financial information. All this information may be used to analyze the quality of care received and to effectively plan therapy in the future. Well-managed records serve as a channel for communication between the treating practitioner and other oral health care experts or clinicians who may be assigned to that patient. Dental records should include enough information for another practitioner to comprehend the patient’s visit to the practice.
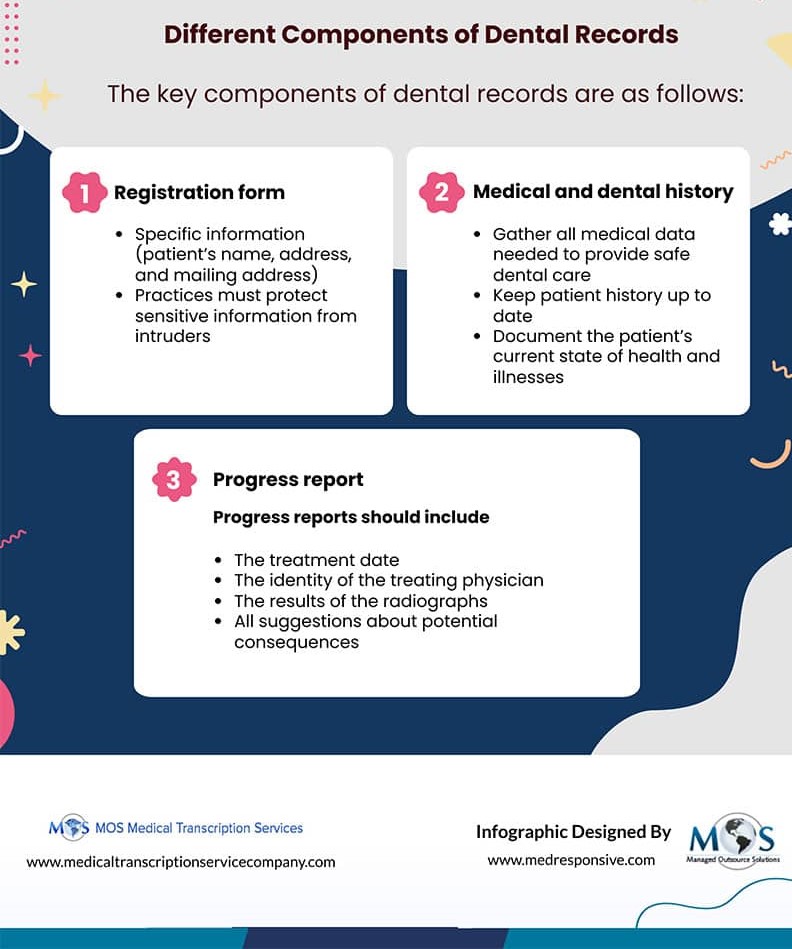
Different Components of Dental Records
The data in the patient chart should be clinical, encompassing all essential patient information, medical history, and encounters with your office and other oral health care experts. The following are key components of dental records:
- Registration form: The registration form asks for specific information such as the patient’s name, address, work, and mailing address, among other things. Due to privacy concerns, a patient’s social security number will not be sought unless the office can demonstrate that it is required to utilize this number rather than an alternative specific identifier issued by the practice. If the office demonstrates a necessity, the practice must be able to protect sensitive information from intruders or computer hackers by blocking or encrypting it. The office will frequently need a Signature on File form if the patient is covered by insurance. When the patient or parent/guardian signs this, it allows billing to insurance without the patient needing to sign each time. This signature can be attached if it is gathered electronically.
- Medical and dental history: Dental professionals must gather all essential and relevant medical information prior to beginning treatment in order to provide safe dental care. Medical and dental histories should be taken in a methodical manner, noting the patient’s current state of health as well as any major illnesses, ailments, or previous adverse reactions that could affect clinical therapy. Any significant dental history, such as an assessment of caries risk and periodontal health, must also be recorded in the patient’s report. Every patient is different, and while planning and sequencing dental care, the dental history should be taken into account alongside the clinical evaluation.
Vital signs can be taken and added to the history once the patient is seated for treatment. When using an automatic machine to take the patient’s blood pressure and pulse rate, as well as their temperature, these can be added to the document. This gives you a chance to talk about the patient’s health in a more private setting.
The dentist is ultimately responsible for keeping the patient history up to date. The patient fills out the medical history form. If the patient is a minor, the parent or legal guardian should fill out the form. The form can be filled on paper or in an electronic format in either scenario and mailed ahead of time if they are on paper.
- Progress report: Progress notes are an important part of the patient’s file. Progress notes should be completed at or immediately after each appointment to ensure treatment continuity, and they must be reviewed and approved by the treating doctor. The level of information necessary varies by patient and treatment, but all progress reports should include the following:
- The treatment date
- A brief yet comprehensive explanation of all services offered
- The identity of the treating physician
- The type, amount, and outcome of any anesthetics utilized, as well as the materials and methods used
- The results of the radiographs
- All suggestions, counsel, and talks about potential consequences or results
Ensuring Dental Record Accuracy
Errors or incorrect information should never be erased or removed from the chart to avoid accusations of tampering. Instead, they should be struck out in a way that preserves the readability of the original notation. Electronic records must be accompanied by an audit trail that achieves the same goal. Entries that are late should be clearly labelled as such. After receiving a claim for compensation or notice of legal proceedings, a clinician should never add to or amend a patient’s chart. Any alterations made in this context would be seen as self-serving, if not outright fraudulent.
Clinical and financial data, as well as radiographs, consultation reports, and medicine and lab orders, must all be kept for a minimum of ten years from the final entry in the patient’s record. These records must be retained for at least ten years after the patient reaches the age of eighteen years in the case of a minor.
The dentist must keep a patient record for all patients who come to the office. He/she should know the medical history of each patient and the condition of their teeth. This will help make the right diagnosis. In addition to this, the dentist must also keep a record of any treatment given to the patient. This will help in fixing the problems that may arise during future appointments.
A reliable provider of dentistry medical transcription services can assist dentists in maintaining an accurate patient record. All dental records can be stored online and accessed whenever required. In addition, it also helps maintain patient privacy as all the data is stored on secure servers with advanced encryption techniques.
![Radiology Transcription Challenges Practices Face [INFOGRAPHIC]](https://www.medicaltranscriptionservicecompany.com/wp-content/uploads/2024/05/radiology-transcription-challenges-practices-face.webp)
![Medical Record Documentation Requirements For Podiatry [INFOGRAPHIC]](https://www.medicaltranscriptionservicecompany.com/wp-content/uploads/2023/05/medical-record-documentation-requirements-for-podiatry.jpg)