
Table of Contents
When every second counts, access to the right information at the right time is crucial. The critical care setting houses patients recovering from major surgery and those with serious ailments or life-threatening injuries. Critical illness or injury is illness or injury that impairs one or more “one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition,” according to the American Medical Association (AMA). Documenting patient information in the critical care environment has an important stake in patient care and safety. Medical reports should be transcribed accurately and in minimum turnaround time. High healthcare documentation quality is critical to deliver timely and appropriate interventions. Medical reports should be transcribed accurately and in minimum turnaround time. However, this can be a challenge in fast paced ED situations. That’s where critical care medical transcription services come in. Experienced transcriptionists can ensure accurate and timely EHR documentation, meeting multiple components for delivering critical care in the ED — while also helping institutions meet critical care documentation standards.
What Critical Care Documentation Includes
Different types of medical reports are generated in critical care units, such as:
- patient progress notes
- vital signs logs
- medication administration records
- laboratory results
- imaging reports
- critical incident reports
- shift change reports
Specific types of reports include:
- Critical incident report: Documentation of any unexpected or potentially harmful event, including medication errors, equipment malfunctions, or falls, to identify areas for improvement.
- Shift change report: A concise summary of a patient’s current status, including vital signs, recent interventions, and planned care, given to the incoming healthcare team.
- Specialty assessments: Depending on the patient’s condition, specific assessments like APACHE (Acute Physiology and Chronic Health Evaluation) or SOFA (Sequential Organ Failure Assessment) scores may be used to monitor organ function and overall severity of illness.
Key Aspects of Critical Care Records
Critical care Electronic Health Record (EHR) documentation of patient information in intensive care units (ICUs), emergency departments, and other high-acuity settings plays a vital role in patient safety, clinical decision-making, and compliance with healthcare regulations. The key aspects of critical care reports are:
- Timeliness:Accurate and timely documentation is crucial for rapid decision-making.
- Clarity and conciseness:Reports should be easy to understand and readily accessible to all healthcare team members.
- Standardized format:Using a standardized reporting system ensures consistent information capture and facilitates comparison across patients.
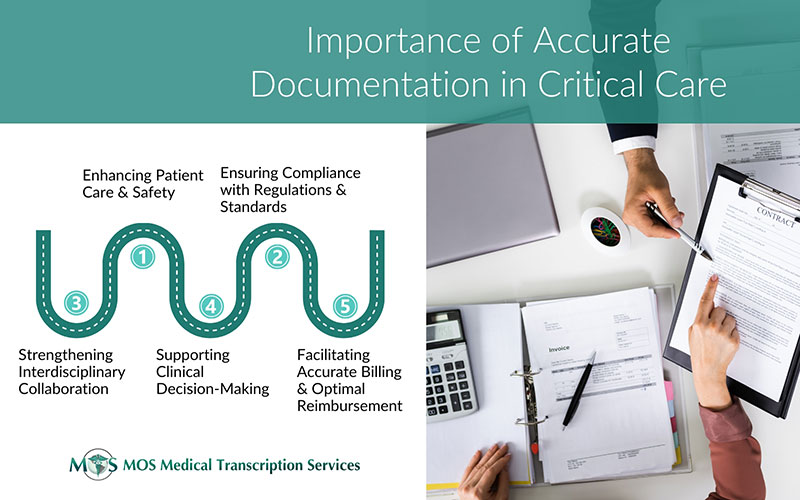
Why Quality Critical Care Documentation Matters
Quality documentation in critical care is the foundation of safe, effective, and responsive care in high-acuity settings. From supporting urgent clinical decisions to enhancing communication among care teams, accurate and timely documentation helps ensure that every patient receives the best possible treatment. It is essential for ensuring patient safety, effective clinical decision-making, regulatory compliance, and optimal reimbursement.
Patient Care and Safety
Critical care patients require continuous monitoring, and precise documentation ensures timely interventions. Accurate recording of vitals, medications, and procedures minimizes the risk of medical errors. Clear documentation supports effective communication between healthcare providers and improves critical care note-taking.
Clinical Decision-Making
Quality documentation provides a comprehensive view of the patient’s condition, helping clinicians make informed decisions. Real-time access to lab results, imaging, and treatment history aids in diagnosing and managing critical conditions. Structured notes help providers identify trends and anticipate complications.
Compliance with Regulations and Standards
Adhering to the critical care documentation standards of CMS, The Joint Commission, and other regulatory bodies is crucial for legal protection. Proper documentation supports quality reporting programs such as MIPS (Merit-Based Incentive Payment System). Clear records protect healthcare providers in cases of legal disputes or malpractice claims.
Accurate Billing and Optimal Reimbursement
Critical care services often involve complex billing requirements. Detailed documentation ensures proper coding and prevents claim denials. Time-based documentation (e.g., for ventilator management or sepsis treatment) is necessary for justifying higher reimbursement levels. Insurance providers rely on detailed records to verify the medical necessity of ICU treatments.
Interdisciplinary Collaboration
Critical care teams, including physicians, nurses, respiratory therapists, and pharmacists, depend on well-documented patient data to coordinate care. Standardized documentation formats ensure that all team members have a shared understanding of the patient’s status. Efficient documentation reduces communication gaps and enhances care transitions.
Improving patient outcomes with better critical care documentation means fewer errors, faster interventions, and enhanced recovery — all of which are vital in life-threatening conditions.
Outsource Transcription for Quality Critical Care Documentation
Outsourcing critical care transcription ensures documents and reports that are accurate, standardized and completed in custom turnaround time. Trained and experienced transcriptionists handle the transcription process, ensuring proficiency in medical terminology, industry-specific style, punctuation, and grammar. QA managers meticulously review and edit transcribed documents, comparing them against the original dictation to enhance accuracy and clarity. Outsourcing reduces the documentation burden and frees up clinicians to focus on patient care. By utilizing structured templates, voice recognition, and AI-powered tools, a medical transcription company can streamline documentation and reduce the workload on clinicians.
Outsourcing reduces the documentation burden and frees up clinicians to focus on patient care. By utilizing structured templates, voice recognition, and AI-powered tools, a medical transcription company can streamline documentation and reduce the workload on clinicians.
Furthermore, the need for standardized critical care documentation procedures is increasingly recognized as a cornerstone of hospital quality and compliance. Partnering with expert transcription providers ensures consistency in note-taking, reporting, and communication among care teams.


