The Centers for Disease Control and Prevention (CDC) recently updated their interim guidance for healthcare professionals evaluating and treating post-v conditions. Despite the varied nature of these conditions, CDC staff has agreed that most of them can be diagnosed and managed by primary care physicians in a patient-centered medical home model. The patients should be examined in four stages, starting 4 weeks after a patient’s COVID-19 infection because some symptoms improve or resolve within 4 to 12 weeks.
According to Jennifer Chevinsky, MD, of the CDC, symptoms that last more than 3 months need specialist referrals or referral to multidisciplinary COVID-19 care centres. Chevinsky suggested a conservative diagnostic approach for the first 4 to 12 weeks. According to her, some patients may need diagnostic testing but lab tests may not distinguish post- COVID-19 conditions. Moreover, they are not required to diagnose post-COVID-19 conditions. If the symptoms continue for 12 weeks or more, additional testing may be considered.
There is no solid evidence on the utility of imaging for post- COVID-19 conditions, so Chevinsky noted that this should be guided by patient history and clinical findings. More advanced testing like cardiac MRIs may be done in consultation with a specialist.
Post COVID-19 condition of a patient can be improved using established evidence-based symptom management approaches to optimize function and improve the quality of life. Chevinsky pointed out that a comprehensive rehabilitation plan might be helpful for some patients. This plan does not include herbal remedies, supplements etc or any other treatment that patients may have used to treat their symptoms.
In ICD 10, there is as yet no code for post-COVID-19 conditions. So, the CDC has recommended documentation of these conditions using B94.8 (sequelae of other specified infectious and parasitic diseases).
Alexis Vosooney, MD of the American Academy of Family Physicians, emphasized the importance of confirming the patient’s experiences, which CDC also recommended in its guidance. She also requested clinicians to talk to the patients about their goals, whether they are looking for an “answer” to their symptoms, to get back to where they were before COVID-19, or whether they have a fear of another disease process. She also added that being transparent with the patient is important and admit that there isn’t much evidence about COVID-19 symptoms and recovery.
Another important aspect is that physicians should be able to distinguish between COVID-19 and other chronic diseases. For instance, shortness of breath need not be because of COVID-19, it could be asthma. Michael Saag, MD, of the University of Alabama at Birmingham, stressed the importance of differentiating between post-COVID-19 symptoms and post-intubation syndrome in patients who were on a ventilator.
Post COVID-19 conditions can be severe, mild or asymptomatic and it can happen to patients, from children to adults, and can be continuing, recurrent, or new symptoms can develop over time. In such cases, it is important to record all these symptoms because it helps physicians study and understand post COVID-19 conditions and how to provide optimal care.
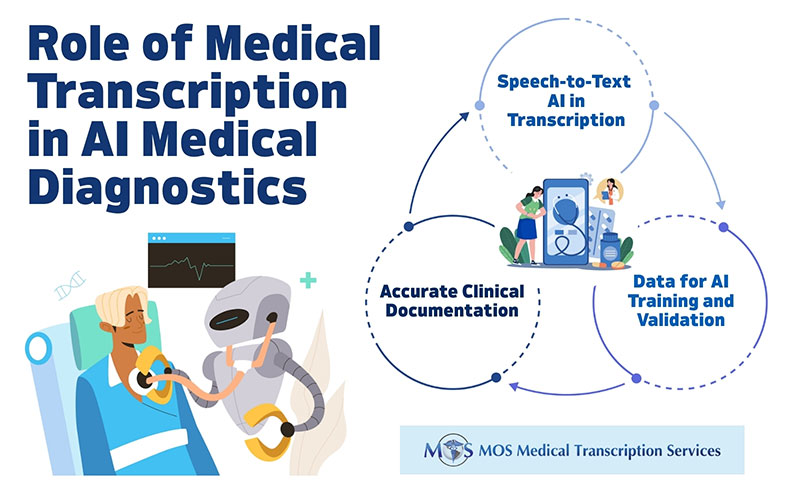
As a company providing medical transcription services, we know how important documentation is in this regard. Accurate medical records are vital to study various medical conditions, treatments provided and patients’ response to those and the outcomes, and so on. The medical documentation should include complete details of the patient, and accuracy in patient records determines the quality of service provided to the patient.