In mental health care, every word matters-and so does how it’s recorded. Accurate mental health documentation is more than a routine practice; it’s a lifeline that supports better diagnoses, safer care, and stronger patient relationships. Even the smallest detail can influence treatment decisions. However, capturing every detail during fast-paced sessions can be challenging for even the most experienced professionals. That’s where advanced AI-integrated medical transcription services can make a powerful difference.
Thanks to modern speech-to-text technologies, the documentation process is now smoother, smarter, and far more efficient than ever. By transforming spoken interactions into clear, structured records, advanced transcription solutions take the weight off clinicians’ shoulders and reduce the risk of errors.
This post explores why accurate documentation is important in mental health care and how working with an experienced medical transcription company can support the process.
Significance of Accurate Mental Health Documentation
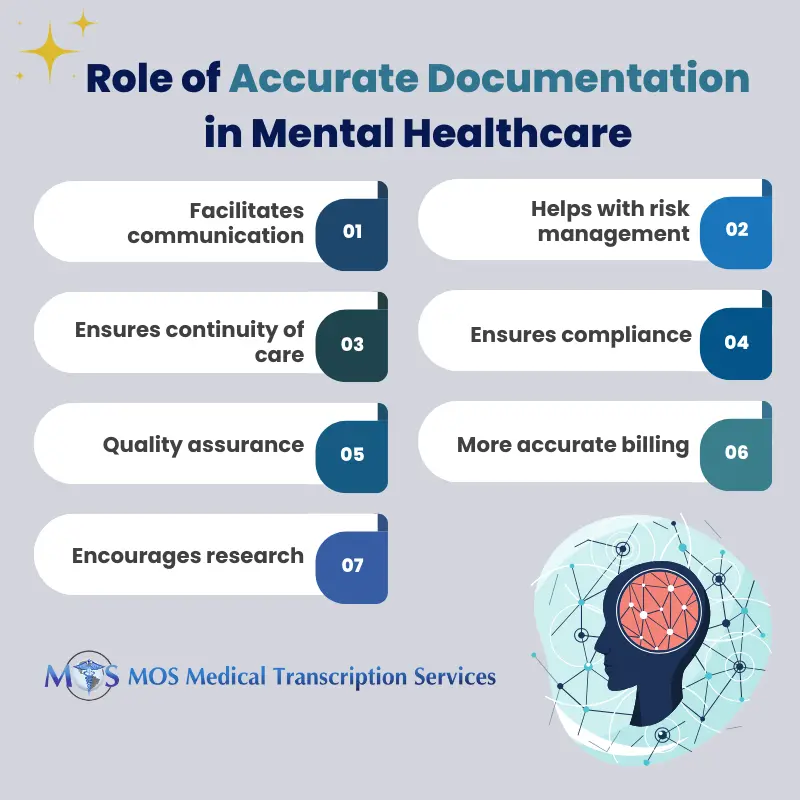
Accurate mental health documentation plays a vital role in the delivery of high-quality, safe, and effective care. Beyond recording patient details, mental health records support effective communication, ensure patient safety, guide treatment planning, maintain compliance, and enable continuous improvement. Effective clinical documentation in behavioral health ensures that every part of the patient’s journey is recorded responsibly. Here’s a clear breakdown of why accurate documentation matters so much in mental healthcare.
- Communication
Accurate documentation is the primary source of truth in mental healthcare. It provides an objective record of a patient’s condition, symptoms, progress, and the care they receive. As mental health treatment often involves a team-therapists, physicians, nurses, and social workers-clear documentation ensures everyone stays informed.
Timely, accessible, readable, and standardized notes make collaboration easier. Providers can quickly understand a patient’s history, previous interventions, and ongoing needs. This shared understanding strengthens communication and improves the continuity of care across multiple professionals and treatment settings. Consistent documentation also improves therapy progress notes accuracy, which is essential for coordinated care.
- Risk Management
Accurate documentation also protects providers in situations involving legal scrutiny. Detailed clinical notes serve as evidence of a provider’s professional judgment and the steps they took to ensure patient safety.
For example, if a patient claims that their therapist failed to identify signs of worsening mental health or potential self-harm, the therapist’s detailed records become crucial. These notes can demonstrate that proper assessments were conducted, risks were evaluated, and appropriate actions were taken. Thorough documentation significantly reduces liability and supports ethical, defensible practice.
- Continuity of Care
In mental health, care is often long-term and may involve multiple professionals over time. When a patient switches therapists, accurate records help the new provider understand the full picture.
These records offer insights into diagnoses, medications, therapy methods used, progress made, and challenges faced. With this information, the new provider can identify what worked well and what didn’t. This leads to informed decisions, smoother transitions, and more personalized, effective treatment moving forward.
- Compliance
Maintaining accurate records is not just good practice-it is required by federal and state laws. Mental health professionals must document the services they provide in a way that clearly reflects medical necessity and aligns with regulatory standards.
For example, Medicaid requires behavioral health documentation that:
- Meets state-specific Medicaid program rules
- Demonstrates the clinical rationale for treatment
- Shows active treatment, including face-to-face time with the patient
- Fully describes assessments, treatment plans, and discharge planning
Accurate documentation also supports ethical practice. By consistently recording informed consent, providers reduce risks related to fraud, waste, and abuse, while ensuring legal compliance.
- Quality Assurance
High-quality documentation helps providers track treatment progress and evaluate the effectiveness of interventions. When clinicians record symptoms, behaviors, progress markers, and patient feedback, they can analyze trends over time.
These insights help:
- Identify patterns in patient behavior
- Understand which approaches are working
- Adjust treatment plans for better outcomes
- This continuous review process leads to more personalized care and helps providers deliver evidence-based, outcome-driven treatment.
- Billing
Accurate documentation is essential for insurance billing and reimbursement. Insurance companies rely on detailed notes to confirm medical necessity and determine coverage.
Mistakes-such as missing information, vague notes, or incomplete records-can lead to denied claims. These errors require time-consuming corrections and resubmissions, which delay payment and disrupt workflow. Thorough, consistent documentation protects both the provider’s revenue and the patient’s access to care.
- Research
Accurate records also support mental health research by providing high-quality data for analysis. Researchers can use documented information-such as symptoms, outcomes, and patient communication patterns-to study mental health trends.
Advanced tools like sentiment analysis can examine emotional patterns in patient speech. When combined with clinical records and other data sources, these insights help researchers better understand psychiatric conditions and develop more effective treatment approaches.
From enhancing communication and reducing risks to supporting continuity, compliance, billing, and research, well-maintained records shape every part of a patient’s therapeutic journey. But the depth and complexity of these sessions make the transcription process more challenging compared to that of other medical specialties. This is why many mental health professionals rely on medical transcription services to streamline the process, reduce errors, and save valuable time that can be reinvested in patient care.
By embracing advanced transcription support, clinicians can maintain accurate therapy and counseling records with ease, ensuring every patient receives the thoughtful, informed, and consistent care they deserve.