Table of Contents
Electronic medical records (EMRs) act as a centralized repository for patient information, including clinical notes, treatment plans, medication records, and billing details. In all specialties, proper documentation is essential for delivering personalized care and monitoring patient progress over time. The golden rule for healthcare providers is: if it’s not documented, it didn’t happen. That’s where professional medical transcription services play a key role. Skilled medical transcriptionists can ensure accurate and timely documentation of a patient’s medical history, diagnoses, and treatment in the EMR, so that physicians have the information they need to diagnose and treat them.
EMRs are designed to improve the efficiency, accessibility, and organization of patient information. However, errors can occur. Minimizing the likelihood of errors in (EMRs is essential for upholding patient safety and high quality healthcare.
Common Errors in EMRs
Here are some common errors in EMRs (Electronic Medical Records) that can impact patient care and operations:
Data Entry Errors: This includes typos, misspellings, or incorrect information entered into fields, improper data formats, and duplicate records or inaccurate patient details.
Incorrect Patient Information: Incorrect patient identifiers, mixed-up records, or outdated details can result in significant medical risks and errors.
Incomplete Documentation: Missing vital clinical notes, treatment plans, or test results and failure to document patient interactions or follow-up care result in inadequate documentation.
Copy-Paste Practices: This refers to overuse of copied text from previous notes, causing outdated or irrelevant information to persist. It also includes lab results, prescriptions, or referrals filed under the wrong patient or category.
Interface Errors: Problems can occur with data synchronization between EMR systems and lab or imaging systems.
Lack of Standardization: Use of non-standardized templates can make records inconsistent or hard to interpret.
Security and Access Issues: Unauthorized access or failure to restrict sensitive data to relevant users, and insufficient encryption increase the risk of breaches.
Overreliance on Automation: This can lead to errors in automated alerts, medication interactions, or clinical decision support tools.
Outdated or Non-compliant Records: This results from failing to update records promptly or maintain HIPAA-compliant documentation practices.
Identifying and addressing these issues is critical to ensuring EMRs effectively support patient care and operational efficiency.
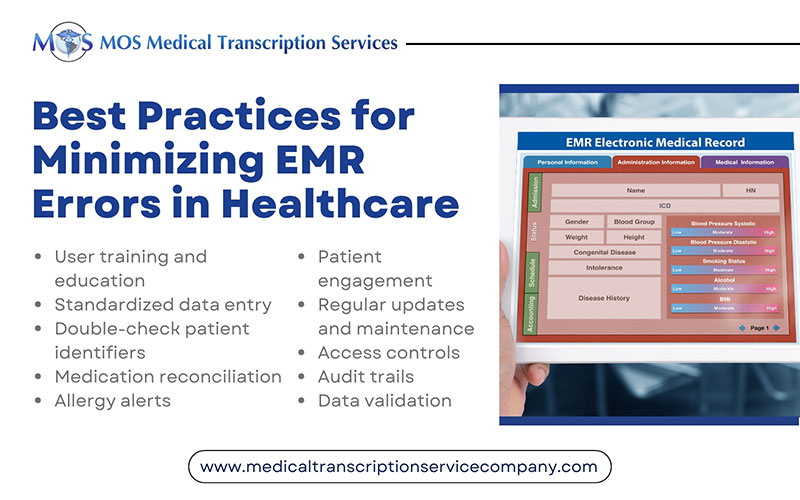
10 Best Practices for Reducing EMR Documentation Errors
Here are some tips to help healthcare providers and institutions minimize the likelihood of errors in EMRs:
- 1. User training and education: Ensure that all healthcare professionals who use the EMR system are adequately trained on its features and functions.Provide ongoing training and updates to keep users informed about any system changes or enhancements.
- 2. Standardized data entry: Establish standardized protocols and templates for data entry to ensure consistency and accuracy.Use drop-down menus, checkboxes, and predefined options wherever possible to reduce free-text entry errors.
- 3. Double-check patient identifiers: Verify patient identities using multiple identifiers (e.g., name, date of birth, medical record number) to prevent mix-ups and duplicate records.
- 4. Medication reconciliation: Implement a robust medication reconciliation process to ensure that medications are accurately recorded.
- 5. Allergy alerts: Configure the EMR to issue allergy alerts and warnings when prescribing medications or treatments that patients are known to be allergic to.
- 6. Patient engagement: Encourage patients to review their electronic records for accuracy and report any discrepancies or errors promptly.
- 7. Regular updates and maintenance: Keep the EMR system up-to-date with the latest software updates, patches, and security enhancements to prevent system vulnerabilities that could lead to errors.
- 8. Access controls: Implement strict access controls and user permissions to ensure that only authorized personnel can access and modify patient records.
- 9. Audit trails: Enable audit trails within the EMR system to track changes made to patient records, allowing for accountability and transparency.
- 10. Data validation: Use data validation rules and algorithms to flag or prevent erroneous entries, such as illogical vital sign values or abnormal laboratory results.
By implementing these best practices to prevent mistakes in electronic health records and fostering a culture of vigilance and accuracy, healthcare providers can significantly reduce the risk of errors in electronic medical records, leading to safer and more effective patient care.
However, a high EMR documentation burden can significantly contribute to medical errors, as the pressure to quickly document patient information can lead to rushed entries, missed details, and inaccurate data, ultimately impacting patient care quality. Outsourcing medical transcription is a practical strategy for preventing medical record errors. By implementing transcription best practices for EMRs, service providers alleviate the documentation burden by ensuring accurate transcription of patient information from physician dictations by trained professionals. This not only ensures precise and complete records but also frees up healthcare providers to focus on patient care, reducing the risk of errors associated with rushed EMR entries.