Table of Contents
Rising levels of burnout among physicians is a critical challenge affecting health systems across the country. In a recent athenahealth survey conducted by Harris Poll, an overwhelming 93% of the physicians surveyed said they feel regularly burned out. A recent Fierce Healthcare article refers to physician burnout as “a challenge that’s reaching a crisis point”. While electronic health record (EHR) systems contribute to physician burnout, outsourced medical transcription services including AI-powered solutions, play a key role in ensuring accurate and timely EHR documentation.
Physicians recognize the value of the EHR for patient care but using the system during the office visit negatively impacts patient interactions and work-life integration. In addition to the EHR data entry challenge, there are several external factors that are responsible for physician burnout. Recent studies have expressed concerns on how this can affect access to care, patient safety, and care quality.
Main Causes of Physician Burnout
- Time and work pressures: According to the Minimizing Error, Maximizing Outcome (MEMO) project funded by the Agency for Healthcare Research and Quality (AHRQ), over 50% of primary care physicians report feeling stressed due to time pressures and work conditions. Researchers found that more than 50% experienced time constraints during exams, and nearly a third felt they needed twice as much time. Additionally, nearly a quarter said they needed 50% more time for follow-ups. Factors like chaotic environments, low work control, and unfavorable culture contributed to physician dissatisfaction, burnout, and intent to leave.
- Laws, regulations and standards: Healthcare providers need to comply with various health care laws and regulations. This growing burden of administrative requirements can affect patient care and negatively impact physician morale.
- Healthcare reform and payer policies: Physicians face challenges navigating the evolving landscape of payment systems, which often come with complex rules and processes. Private insurers are increasingly utilizing risk-sharing contracts, which adds significant administrative burden for healthcare providers.
- Medical record documentation and coding requirements: Patient records are vital for assessing a patient’s health condition, planning and evaluating the patient’s treatment and to ensure the best care possible, However, EHRs have specific documentation requirements and on physicians and complying with them can be challenging.
- Quality reporting: Quality measures in medical reporting are vital to ensure accountability, transparency and to deliver increased value in health care. However, there are various performance measures that need to be filled and this adds to physician burnout.
- Prior authorization: Physicians may need to obtain preapproval from payers before prescribing medications, other forms of treatment, diagnostic procedures and referrals. This can make things difficult for providers and patients. Submitting and obtaining prior auth is a complex process, with rules varying among payers.
- Drug monitoring: Physicians use authorized prescription drug monitoring programs to make prescribing decisions, reduce polypharmacy, and avoid supplying opioids to patients that have drug-seeking behavior. However, access to the database differs from state to state, making matters difficult for physicians.
- Professional liability: Obtaining medical licensure requires meeting certain criteria, Despite recent efforts to simplify and standardize the licensing process, physicians are still required to provide detailed information about their physical and mental health as part of their application. This includes answering questions about their health status and any past or current conditions that might affect their ability to practice medicine. The process of disclosing this information can create a barrier to seeking the necessary treatment.
- Patient-physician relationship: The conventional societal value “doctors know best” has changed to a “patient centric model” where physicians and patients build a rapport to create a better medical experience. Although this system is useful for patients, it could lead to deterioration of trust with physicians and the healthcare system.
EHR-related Physician Stress
EHRs (Electronic Health Records) have many advantages for physicians’ offices and hospitals. However, they have also transferred several administrative tasks to physicians, including billing, coding, and electronically prescribing medications. Reports also point out that the focus of EHR systems on documentation for billing purposes can be contrary to effective and efficient documentation of clinical care. This means that EHRs can, in fact, contribute to increased stress and burnout among healthcare providers.
A study titled “Association of Electronic Health Record Design and Use Factors with Clinician Stress and Burnout” found a link between key aspects of EHR design and physician well-being. An article from the American Medical Association (AMA) lists these factors as:
- Information overload.
- Slow system response times.
- Excessive data entry.
- Inability to navigate the system quickly.
- Note bloat.
- Fear of missing something.
- Notes geared toward billing, not patient care.
The lead author of the study, which was published before the pandemic, stated that physicians experience burnout because they are spending so much time on the computer and don’t feel they get enough time to take care of their patients.
So what is the solution? Here are some strategies recommended by industry experts.
Strategies to Combat Physician Burnout
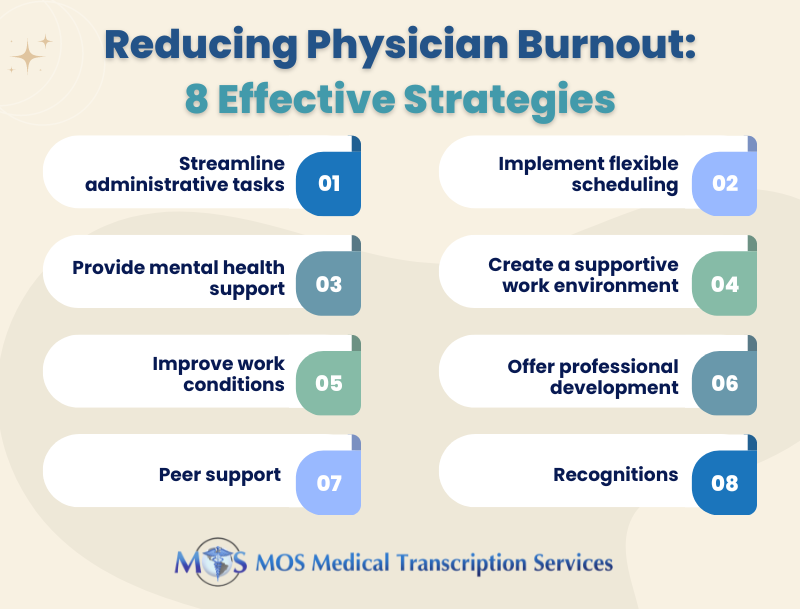
- Streamline administrative tasks: Implement efficient systems and solutions like medical transcription services to reduce the burden of paperwork and administrative duties.
- Implement flexible scheduling: Explore options for flexible work schedules or part-time opportunities to help physicians manage their workload more effectively.
- Promote work-life balance: Encourage physicians to take regular breaks, use vacation time, and establish boundaries between work and personal life.
- Provide mental health support: Offer access to mental health resources, counseling, and support groups to help physicians manage stress and emotional challenges.
- Create a supportive work environment: Create a collaborative and supportive work culture where team members can share responsibilities and provide mutual support.
- Improve work conditions: Implement solutions to improve the efficiency and comfort of the work environment like ergonomic workstations and updated electronic health records systems.
- Offer professional development: Provide opportunities for continuing education and career growth to keep physicians engaged and motivated.
- Peer support: Develop mentorship programs and peer support networks to help physicians share experiences and advice.
- Recognitions: Recognize and reward physicians for their hard work and contributions to the practice.
Today, hospitals and health systems are investing in AI medical scribes and generative AI tools to tackle the burden of administrative tasks that take up so much of clinicians’ time, according to the Fierce Healthcare report. Even so, the support of a medical transcription company remains relevant. Human medical transcriptionists can interpret complex medical terminology and jargon with a level of precision that current AI tools might struggle with, particularly in cases where context or specialized knowledge is crucial.


