Table of Contents
A discharge summary is a valuable document that gives an overview of a patient’s hospitalization from admission through discharge. It provides information about the continuity of care and supports safe patient transition from the hospital setting to another level of care or home. A discharge summary is generated when a patient is discharged from hospital. It contains vital details such as reason for the hospitalization, key diagnostic findings, treatments provided, patient’s health status at time of discharge, medications, care instructions, and follow-up plans. Hospitals are turning to EHR-integrated medical transcription services to ensure accurate and timely discharge summaries.
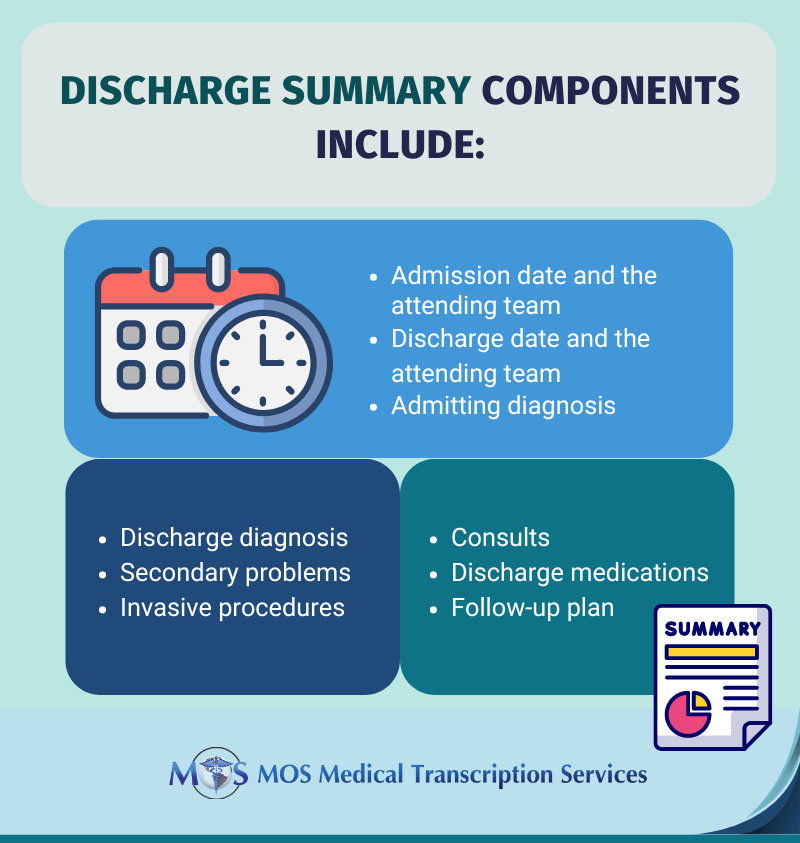
Components of a Discharge Summary
The discharge summary is an overview of the vital aspects of the patient’s care.
Significance of Discharge Summaries often Overlooked, say Studies
According to studies from the Yale School of Medicine studies, detailed discharge summary from the hospital to the patient’s primary care physician can help avoid readmission and aid in the patient’s recovery. Discharge summaries inform the subsequent healthcare provider about the patient’s health status. When the patient is discharged from the hospital, the physician handling the follow-up care should be given an accurate and complete discharge summary.
According Dr. Leora Horwitz, adjunct professor at Yale School of Medicine and director of the Centre for Healthcare Innovation and Delivery Science at New York University Langone Medical Centre, discharge summaries are more often used a tool for billing purposes and not fully utilized as a tool for transitions.
Horwitz’s team analyzed around 1500 discharge summaries from 46 hospitals. The study highlighted the importance of timely and accurate discharge summaries for efficient care post hospitalization. The team’s second study found that the quality of summaries was directly related to the risk of readmission.
The effectiveness and quality of care for patients largely depends on the communication between physicians both in secondary and primary care. Discharge summaries should ideally be completed prior to discharging patients from the hospital and copies should be kept in the patient’s file, given to the patient as well as forwarded to the concerned provider.
Discharge summaries provide clear guidance on how care must be rendered to the patient. Clinicians will have a clear idea of what treatment to administer, when to administer it, and what reaction to expect from the patient. A complete discharge summary is also proof of the care and concern the hospital shows towards the patient and the steps it takes to ensure the patient has a great follow-up.
Incomplete Discharge Summaries Cause Fragmented Care
Lack of a proper discharge summary can cause issues. When patients are transferred without any clear instructions, it can impact patient safety and care, increasing risk of readmission.
Fragmented care and treatment not efficiently coordinated has been one of the major causes of increased healthcare costs and patient harm according to the Health and Medicine Division (HMD). Apparently, even high performing health systems lag behind in the timeliness and transmission of discharge summaries as well as in the content quality. Sharing patient information is a vital aspect of care delivery. Inaccurate or delayed information transfer through the various care levels has a negative impact on re-admission, safety, efficiency as well as other quality dimensions.
Research conducted by the Yale University School of Medicine on heart failure exacerbation patients also found that quick distribution of detailed discharge summary to patients’ physicians improved outcomes following a hospital stay and reduced the chances of them being readmitted within a period of 30 days. In other words, the higher the quality of the discharge summary is, the lower the risk of complications which would necessitate readmission.
Key Elements of Discharge Summaries
The three essential aspects of the discharge summary are timeliness, smooth transmission, and content quality:
- Timeliness is a very important factor. Hospitals must create a summary and provide a copy to the primary care provider in a timely manner. The Yale University School of Medicine research found that nearly 8% of the surveyed facilities did not have discharge summaries ready till 30 days had passed following the discharge.
- Transmission must be smooth. Hospitals should ensure that the summary is prompty sent to the right practice or clinician for the next level of care after discharge. This is crucial to ensure follow-up care.
- Content quality is crucial. Discharge summaries must have important details regarding the condition of the patient during discharge, any pending tests to carry out, further medication to be administered, and other follow-up recommendations.
Flawless Discharge Planning
In line with these factors, it would be wise to evaluate the discharge process of your hospital if there are issues in your discharge summaries. It is important to remember that the preparation for a smooth discharge starts right when the patient is admitted. The AHA (American Hospital Association) has brought out a few guidelines that hospitals must follow regarding discharge planning:
- To begin with, discharge planning must be based on the sound judgment of physicians and other medical professionals involved in the patient’s care.
- It is important to analyze the needs of each patient before deciding on their post-hospital placement following their discharge.
- EHRs need to be utilized to their full capacity for reducing or streamlining any administrative burden that could arise because of thorough discharge planning.
- Clinicians must collect all the required information while the patient is at the hospital to make the right decision regarding post-discharge care.
Physician and hospital documentation can be streamlined and completed in a timely manner with the help of a reliable medical transcription company. Experienced medical transcriptionists can ensure high-quality reports EHR integrated documentation. Accurate and timely discharge summaries will have a positive impact on patient care and reduce readmission rates.


